Any abnormal Immunological acquired reaction (IgE & Non-IgE) to the exposure of Allergen or Antigen, which are normally harmless to individual.

T-helper Cells (TH-1 & TH-2) are the supervisors of the immune reaction. TH-1 cells are immune cells that reject transplants and could, if given free rein, reject a foetus or retard its growth while TH-2 cells produce IgE antibodies (Allergy causing antibodies). So one effect of protecting the foetus from rejection is to push the immune system towards a greater tendency for TH-2 cells, means towards allergic diseases. Normally at birth, there is sudden deviation in immune system (up. regulate TH-1), so new born is healthy but in contrast this process appears to fail in allergic (atopics) patients and moreover, if mother is allergic & environmental factors as:
- Cow’s milk formula feed
- Early intake of solid food
- Highly allergic food
- Antibiotics before 2 years
- Exposure to by products of smoking
- Exposure to indoor allergens like house dust mites etc.
All these provoke the setting of immune system towards TH-2 Allergic sensitization, in the first few months or even before birth. Our first two years of life are more vulnerable to allergens to induce ALLERGIC DISEASES.
The common allergic diseases are :
- Atopic Dermatitis – Itching, reddening and feeling of flaking of the skin.
- Allergic rhinitis – Sneezing, watery eyes and nose, post – nasal drip, nose block, congestion.
- Allergic Conjunctivitis – Itchy, red watery eyes.
- Allergic BR. Asthma – Cough, wheeze, breathlessness and tightness of chest.
- Allergic Rhino – sinusitis – Headache, congestion, throbbing pain in and around the eyes & cheeks, nose block, and post-nasal drip etc.
- Urticaria & Angioedma – ltchy hives and non-itchy swelling of lips, eyes etc.
- Anaphylaxis – a violent allergic reaction to insect, stings, food, drugs and latex.
- Food allergy – induces recurrent Urticaria, Iarynagioedma, Atopic dermatitis, Brittle asthmatic, Anaphylaxis etc e.g. peanut, fish, etc.
- A.B.C.D. (Air-Borne Contact Dermatitis)
- Contact Allergy (chemicals etc)
- Allergic Vasculitis
- A.B.P.A. (Allergic – Bronchopulmonary – Aspergillosis)
- Occupational Asthma
We can spoil our immune system too easily by protecting it from life’s natural challenges and obstacles by change in (food and air quality) life style so called Hygiene hypothesis. Moreover, the following factors promote an allergy-asthma tendency as :
- Exposure to a virus called RSV (Respiratory syncital virus) during infancy, which provokes on lgE reaction.
- Exposure to allergen such as house dust mite and animal danders.
- Taking antibiotics in infancy.
- Breathing No2 (Nitrogen dioxide) from gas stoves and formaldehyde from various household sources. The poor ventilation of many modern houses and the greater time spent indoors aggravates the problem by exposure to irritants.
- Smoking by mother during pregnancy and afterwards
- Abrupt early weaning and or Bottle feeding and early intake of solid foods.
There are two main reactions caused by Allergen / Antigen:
-
Immediate reaction (IR)
– It involves mast cells and IgE antibodies. There are two specific IgE antibodies for the allergen on the mast cells and the allergen has to bind to both these specific IgE antibodies, so it forms a link on mast cells to degranulate its pharmacological active substances like histamine into the blood. As mast cells are plentiful in the lining of the nose, airways, skin and digestive tracts, so histamine like substances causes reactions:
- In the airways – Contraction of smooth muscle (bronchospasm)
- In the skin- Increased leakiness of the smallest blood vessels into surrounding area (Urticaria and Angioedma)
- In the Nose & eyes – Capillary permeability and widening of blood vessels (Rhino – congestion)
- Excessive release of histamine into blood – a drastic fall in blood pressure (hypotension) due to widespread opening of blood vessels and leakage of fluid into the tissues e.g. anaphylaxis.
-
Late Phase Reaction (LPR)
– This reaction starts(1-2 hrs ) hours after exposure to the allergen and last about 24 hours. It involves different type of immune cells – eosinophils and lymphocytes. Infact, eosinophils are major aggressive cells. They can release toxins like ECP and M.B.P. (Eosinophilic Catanoic protein and major basic protein) responsible for inflammation of allergic diseases.
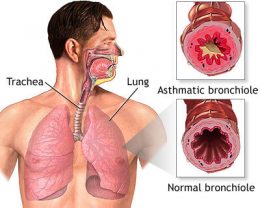
It is a complex inflammatory disease, where there is a basic defect in immune system and disturbance in autonomic nervous system. Clinically presenting as generalized airway obstruction paroxysmal in nature, respond either spontaneously or with bronchodilators. Physiologically diagnose on the basis of variability and reversibility >15% with bronchodilators by spirometry and peak expiratory flow meter. Immunologically – inter – play between the mediators of cells (mast cells, eosinophils and lymphocytes and neuro – transmitters,) which leads pathologically as airway edema, hyper reactivity, infiltration of inflammatory cells predominately eosinophils, epithelial cell damages, & shedding, Hyper-plasia of airway smooth muscle. Sub epithelial fibrosis and ends in fixed airway obstruction.
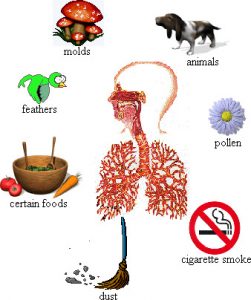
Allergens and viral respiratory infection shifts the immune system towards TH-2 cells, common allergens include plant pollen (tree, grass, and weed) house-dust mites, molds, animal danders, insects and certain foods, etc.
Aspirin and tartazine, cold air, smoke, industrial chemicals, perfume, paint and gasoline fumes as irritants, Sulfites as food additives and preservatives causes’ asthma attack.
Dust mites & Asthma:
House dust mites are the main causes of Allergic-Asthma, fount in house dust. Mites live in beds, carpets, upholstery and stuffed toys. Mites prefer warm and moisture; it is the faecal part of house dust mite which is highly allergenic and initiates the plasmin induced activation of photolytic Enzymes.
The clinician’s investigation of the allergic patient has two components:
- Evaluation of the patient’s environment.
- Evaluation of the patient’s immunologic response to allergens. Once the triggers are identified, the treatment strategies can be formulated, before any therapy is instituted, the suspected allergen must be identified.
We define Atopy (or) Allergy reaction as specificity against specific peptides. The peptides may be present either in foods or in aero-allergens. It is the cumulative effect of the total intake of peptides, which enters into our body responsible for symptomatology. As IgE -antibodies does not look at whole antigen / allergen molecule but simply recognizes a characteristic cluster of chemical features called Peptides, which induces cross reaction. These peptides may behave like close cousins as in house dust mites, storage mites contains presence of tropomyosin found in dust mites and shrimps fish, presence of paralbumin in all kind of fishes and or ovalbumin in eggs of all birds, peanuts and legumes (The bean and pea family-leguminosae) have homologous peptides, induces cross – reactions in body.
- Allergic diseases like bronchial asthma, allergic rhinitis, and atopic dermatitis are increasing dramatically.
- Major causative agents implicated are pollens, fungal spores, dust mites, animal epithelia etc.
- Upto 30% of all visits to general practitioners and paediatric specialists are due to allergic symptoms.
- Lack of awareness forces people to deal with the problem symptomatically.
- Allergic diseases, if not detected early, can lead to severe Consequences.
Allergy is the cause, while Asthma is the effect of Allergy reaction on the lungs. Not all asthmatics are allergic and there are many people who are allergic but do not have asthma.
Asthma & Allergic rhinitis (one airway, one disease) have well documented relationship as 60% of asthmatic patients have associated rhinitis.
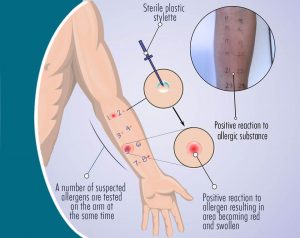
The principle behind the allergy testing is to detect the allergic reaction to the various groups of allergens by skin prick test, intradermal test, prick- puncture test. It is also an indirect measurement of specific IgE Strongly positive tests is indicative of sensitzation as well as the inflammation by the specific allergen early and late reaction. As all of these allergens are typically made of protein, allergy testing detects which of these proteins are highly sensitive to patient. History & Immunological-significant positive skin test, specific lgE with high absolute esnophil count and positive challenge test are the best predictors to diagnose allergic asthma disease. Age should not be considered the limitation for skin prick test as presence of allergic sensitization specially to house dust mite and alternaria is a potential risk factor to detect and development of the early diagnosis of bronchial asthma in a recurrent cough – wheeze – syndrome in a child.
Immunotherapy is the repeated administration of specific allergen to patients with IgE – mediated conditions to provide protection against the allergic symptoms & inflammation. Now a day’s standardized product of allergens are used in clinical practice of allergen-Immunotherapy & we are at the corner to administer recombinant allergens therapy to suppress TH-2 lymphocyte activity. Initial work on mechanism of Immunotherapy was focused on circulating antibodies but now most studies are on T-cell response. Immunotherapy acts either by immune deviation (increase THO /TH1) or T cell energy (decrease in TH2/THO) or more likely both. Immunotherapy affects the natural course of disease & increases systemic and local increase in CD8 T regulatory cells.
- Subcutaneous Immunotherapy
- SLIT (Sublingual Immunotherapy)
- RIT (Rush Immunotherapy)
- CIT (Cluster Immunotherapy)
- Anti-IgE (xolair) Therapy
- Oral Desensitization
- Aspirin Desensitization
- Chemical & Drugs Tolerance
The basic difference between Specific Immunotherapy & drugs are that specific Immunotherapy (SIT) results in long term remission of disease while the drugs treatment has to be continued for life long. Immunotherapy is effective several years even after discontinuation, which is not due to decrease recruitment of inflammatory cells, (masts cells & Eosinophils which has short half life), but is due to modified synthesis of allergen specific T regulatory cells which is not possible with the present drugs therapy. We must however realize that drugs treatment alone does not seems to solve the prevalence of allergic- asthma diseases, until or unless, we are able to interfere with a etiological caustic factor.
Specific Immunotherapy is the only potential curative treatment as it interferes with the patho-physiological mechanisms of the disease. The better the patient understands the disease & the potential for intervention, better the chances are of obtaining a good result which will increase the patient compliance & improve the quality of life. So a single modality like drugs therapy will not be as effective as interference at different levels as allergen avoidance & specific Immunotherapy cascade.
-
Patient compliance –
The actual efficacy of drugs in clinical practice is only 50 % either the patient does not take drug or take it intermittently or in a reduced dose.
-
Clinical efficacy –
Though inhaled corticosteroid is effective, but complete freedom from symptoms is not the rule. Unless we prescribe high dose 800ug as for cellular inflammation & 1200ug for suppressing the mediators & cytokines.
-
Long term side effects of ICS –
In general the use of topical steroids is considered to be safe. One side effect that I.C.S. have a systemic effect is the high frequency of easy brusing which is not always reflected in hypothalamus – pituitary adrenal (HPA) function The current trend to use ICS in larger doses in young patients calls for some caution in view of our lack of knowledge with long term use for more than 30 years of ICS & their relation in preventing the accelerated decline of. Lung function Test (FEV1).
-
Uncertainty of drug delivery of ICS –
BR asthma is complex infllammatory diseases of air ways as inflammation also involves mucosal membrane of small airways, so there is risk of development of chronic irreversible & structural changes in the small airways because of uncertainty of delivery of ICS in peripheral airways as lung function PEFR/FEVI only measure large airways function & do not indicate the true state of inflammation of lower Peripheral airways.
Normally in healthy subjects, T-cell response to allergens entering the mucosal route is actively suppressed by IL-10 (INTERLUKIN –10) &TGF- B (Transforming growth factor –b) while this T cell response is less in allergic- asthma patients, so principle behind successful Immunotherapy (SIT) is to generate T -regulatory T-cells of CD4 +/CD25 +Type which secrete IL-10 & TGF-B. Indeed, IL –10 is able to generate non – inflammatory IgG4 antibodies by memory B cells & TGF –b acts as a switch on & promoting factor IgA. Both cytokines suppress IL4- IgE inflammation &IL5 – Eosinophils infiltration. (TGF –b & IL -10 = IgA & IgG 4 =)
IL –10 on TH-2-It is a major Immunoregalatory cytokine
- IL –10 plays an important role in the cross- regulation of the TH1 & TH-2 cytokine
- It prevents antigen presenting cell (APC) dependent IgE synthesis
- It inhibits IgE dependent cytokine- release from mast cells.
- It inhibits IL –5 syntheses by resting CD 4+T cells as IL –5 is a key event in the induction of eosinophilic infiltration & airway hyper responsiveness
- It also suppress the lipo- polysaccharides ( LPS )induced generation of GM – CSF & TNF & by eosinophilic & consequently accelerates eosinophilic death, IL –10 induces a long term antigen specific anergic state in human CD4+/ periphery T cells & regulates allergen specific IgE & IgG production by B cells in favor of IgG 4
Why IgE antibody takes several years of treatment for its reduction is due to delayed synthesis of T cell cytokines for priming, survival & activation to suppress allergen inflammation by mast cells basophiles & Eosmnphils.
TGF-b ON TH2 – It is secreted by regulatory T cells & other immunologically active cells
- It can Inhibit B- cell proliferation antibodies production & expression of surface molecules including antigen receptors
- It plays an important role in mucosal immune response & has been implicated in the induction of class switch & secretion of IgA
- It also inhibits MCH-II expression on monocrytes
- It has a regulatory function in human airway & prevents inflammation in responses to aeroallergens .& maintain the harmonious bronchial architecture
It has been shown that oral Immunotherapy generates antigen specific TGF-b secreting regulatory T cells. Which localize to the target organ & suppress inflammation in the local microenvironment?
Current evidence suggests that Immunotherapy modulate T cell response to allergen either through immune deviation to a TH –1 response or though induction of a modified TH-2 cells or regulatory T cells response with high IL-10 & TGF –b secretion .SIT is the only curative approach for specific IgE mediated diseases.

John Freeman coined the term “rush” derived from the relative speed at which allergen Immunotherapy shots are administered or multiple injections on oneday or frequently on multiple days in a row. John Freeman initially started eight injection per day, but now some centers are administering four injection at hrly interval for five days in adults & 3 injection daily at 2 hourly interval for five days in children. Once maintenance tolerance doses (MTD) is achieved, subsequent injection are given weekly for three injection then biweekly for three injection
- Patients with asthma must have spirometry or peak flow measurement before 30 mts and 60 mts after each injection, Immunotherapy is to be given only if FEV1 more than 70 % of predicted value, or PEFR is greater than 80 % of predicted value.
- Patient with asthma should continue to take all their scheduled medication those requiring daily asthma therapy should be considered for administration of glucocorticosteroids (0.5 mg /kg) each morning one hour before the first injection from the two most concentrated vials (to diminish the likelihood of a late asthmatic reaction, if they experience a bronchoconstrictive reaction to the injection on that day)
- Patient is to remain within view of the nursing staff and with a physician available for 60 minutes after each injection.
- In addition to FEV1 or PEER, patient will have pulse and blood pressure determined before Immunotherapy and repeated should they complain of any symptoms after the injection.
- The site of the injection will be examined at 30 minutes and the size of the reaction recorded
- Check label carefully to be certain that the correct patient’s extract and correct concentration are being
- Shake the bottle before use
- Use a tuberculin syringe and 26 or 27 gauge needle give injections subcutaneously in the poster lateral surface of the middle third of the upper arm. Staying away from the joints always pull back the plunger before the allergen extract is administered ,if blood returns , withdraw the needle and use the other arm
- Rotate injection sites
- Do not massage the injection site.
- Record dilution, dose reaction, and FEV1 or peak expiratory flow rate (PEER) for each injection on the Immunotherapy dosing record
- Local reaction greater than 3cm indurations – repeat the same dose, greater than 7cm or persisting over 12 hours from time to injection -reduce one dose
- Mild systemic symptoms (rhinitis , mild asthma) -return to previous dose – consider 2 hours interval
- Generalized systematic reaction – decrease by two dose – consider 2 hour dosing interval
- Take ANTHITAMINE (cetrizine / clamist) oral steroids. (wysolone / medrol if local reaction > 12cm)
- Always use inj Adrenaline (0.3 –0.5 ML) If there is h/o sneezing / anaphylactic reaction after Allergy shots
Once the maintenance dose is reached the frequency of injection is gradually reduced a guideline for reducing the interval of injection is :
- Every week x3 (do not exceed 7 days for maintenance injection)
- Every 2 week for 2-3 injection
- Every 3 weeks for 2-3 injection
- Every month maintenance dose for 3 years duration of Immunotherapy
